What are Varicose Veins of Leg?

Introduction
Varicose Veins are the superficial veins of the limbs which becomes dilated, elongated and tortuous
Surgical Anatomy of Varicose Veins of Lower Limb
A) Deep Veins: Deep veins of lower limb shows numerous arteries and branches with there respective valve
- Posterior tibial veins and its tributaries
- Peroneal vein
- Anterior tibial vein
- Popliteal vein
- Femoral vein
B) Superficial Veins: Superficial veins lies in the subcutaneous fat between the skin and deep fascia
- Long (Great) Saphenous vein and its tributaries
- Short (Small) Saphenous vein and its tributaries
C) Perforating or Communicating Vein: These veins communicate between Superficial and Deep veins, which are of following two types
- Indirect Perforators
- Direct Perforators - in the leg, knee and thigh
Etiology of Varicose Veins of Leg
- Morphological Factor: Erect posture against gravity
- Congenital cause
- Prolonged standing: On prolong standing long columns of blood puts pressure on weak valves of veins, which causes failure of veins giving rise to varicosity of long or short saphenous vein
- Obesity: Excessive fatty tissue in the subcutaneous tissue offers poor support to the veins, leading to formation of varicosity
- Pregnancy: Progesterone causes dilation and relaxation of veins, which makes valves incompetent, along with that in pregnancy uterus causes pressure on inferior vena cava causing obstruction of venous flow
- Old age: It causes atrophy / weakness of venous wall and veins gradually becomes incompetent with age
- Athletes: Forced contraction of calf muscles forces the blood through perforating veins in reverse direction, causing destruction of perforating veins and ulitimately leading to formation of Varicose Veins
Clinical Features of Varicose Veins of Leg
- Tired and aching sensation in affected lower limb at the end of day
- Sharp pain in grossly dilated veins
- Cramps in the calf shortly after retiring to bed
- Pain may be bursting or severe in nature particularly localized to the site of incompetent perforating veins
- Swollen ankles in evening
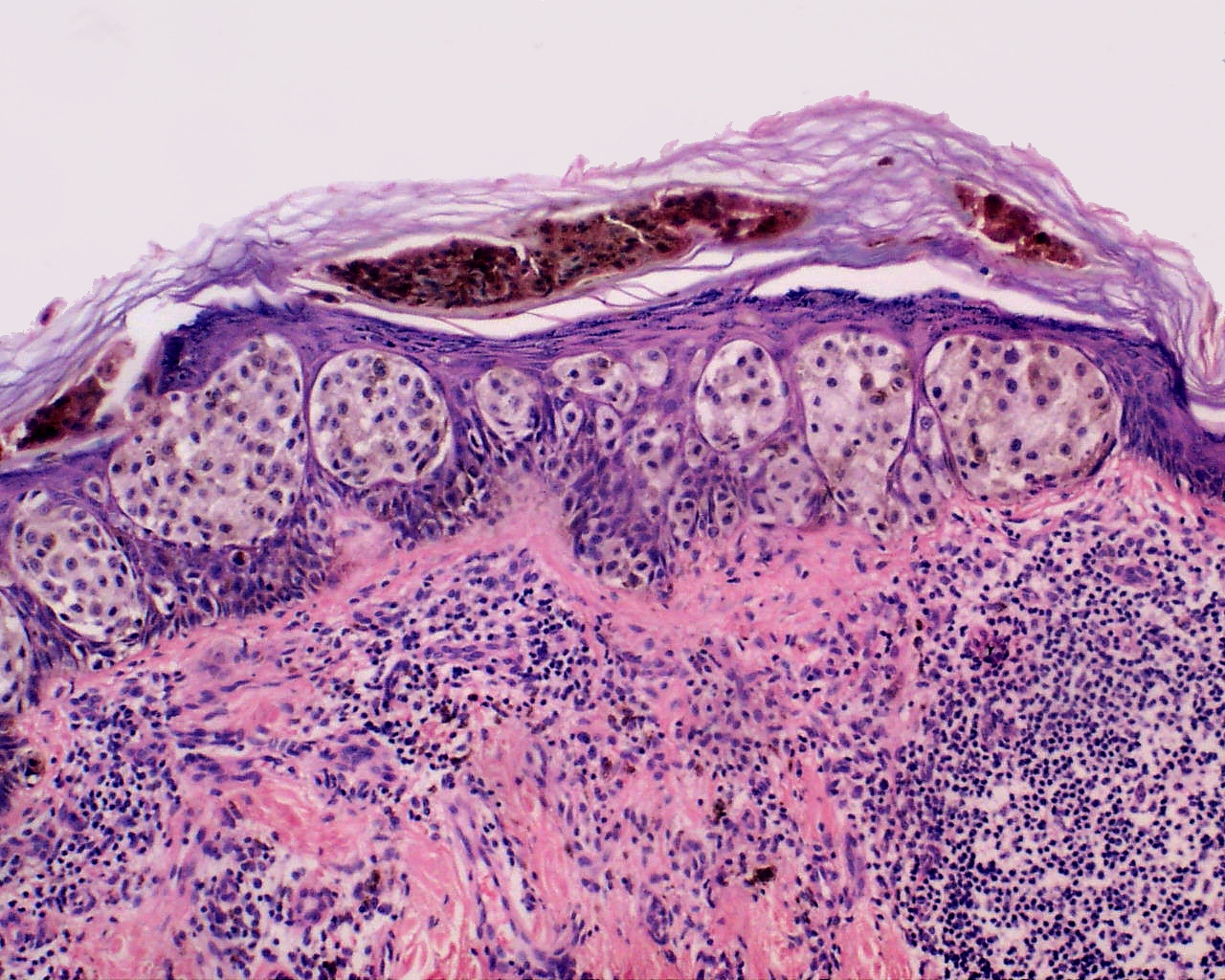
- Itching and pigmentation over varicosed skin
- Eczema of affected skin
- Venous ulceration
Local Examination of Varicose Veins of Leg
A) Inspection:
- When patient stands up veins becomes prominent
- One can feel characteristic thrill when patient coughs
- Varix disappears when patient lies down
- When the varix is tapped with fingers, a fluid thrill obtained in long saphenous vein
- Examination of Venous Ulcer
B) Palpation: Dilated veins are palpated, presence of Cough Impulse is elicited and following tests can be performed
- Brodie-Trendelenburg Test - for Sapheno-Femoral valve incompetence
- Pratt's Test
- Modified Perthe's Test - for deep vein thrombosis
- Schwartz's Test - for superficial column of blood
- Morrissey's Test / Cough Impulse Test - for Sapheno-Femoral valve incompetence
- Fegan's Method - to indicate sites of perforation
- Multiple Tourniquet Test - for perforator incompetence
C. Other Examinations includes following:
- Abdomen examination - to rule out Pregnancy, Inferior venacaval obstruction eg. Thrombosis
- Vaginal or Rectal examination to rule out pelvic tumors
- Peripheral arterial pulse examined to exclude presence of arterial insufficiency
Special Investigation of Varicose Veins of Leg
- Ascending Phlebography
- Thermography
- Radioisotope Scanning
- Radioactive Fibrinogen Studies
- Venography - Ascending and Descending
- Doppler Ultrasound
- Photoplethysmography
- Duplex Ultrasound Imaging
Treatment of Varicose Veins of Leg
- Palliative Treatment
- Avoidance of prolonged standing
- Creep bandage or elastic stockings are worn throughout the day from toes to thighs, only taken off during sleep
- Limbs should be raised above the heart
- Exercise like bicycle riding in the air while lying on the bed, walking etc. should be done to strengthen the calf muscles
- Operative Treatment:
- Indicated for Positive Trendelenburg test and Sapheno-Femoral Incompetence
- Contraindicated in Pregnancy,Thrombophlebitis and Women taking contraceptive pills
- Ligation
- Ligation and Stripping
- Multiple Cosmetic Phlebectomy
- Post-Operative Management
- Fegan's Injection and Compression Treatment